Scientific update on the use of masks to prevent the spread of Covid-19.
In a recent article from researchers at UC Davis the scientific evidence of facial masks helping to mitigate the spread of COVID-19 was reviewed. The conclusion is that scientific evidence is clear: Social distancing and wearing masks help prevent people from spreading COVID-19, and masks also protect those who wear them.
A range of new research on face coverings shows that the risk of infection to the wearer is decreased by 65 percent, said Dean Blumberg, chief of pediatric infectious diseases at UC Davis Children’s Hospital.
Let’s look at some basic science.
The new coronavirus, SARS-CoV-2, is tiny, about 0.1 microns – roughly 4 millionths of an inch – in diameter. They are easily carried within respiratory droplets of various sizes. Respiratory infections can be transmitted through droplets of different sizes. While the respiratory particles are also tiny they are much larger than the virus itself. When the droplet particles are >5-10 μm (μm= micron, there are 10,000 microns in a centimeter) in diameter they are referred to as respiratory droplets, and when they are <5μm in diameter, they are referred to as droplet nuclei, another name for respiratory particles. According to current evidence, COVID-19 virus is primarily transmitted between people through respiratory droplets and contact routes. Droplet transmission occurs when a person is in in close contact (within 6 feet) with someone who has respiratory symptoms (e.g., coughing or sneezing) and is therefore at risk of having his/her mucosae (mouth and nose) or conjunctiva (eyes) exposed to potentially infective respiratory droplets. Transmission may also occur through fomites (a contact surface like a door handle) in the immediate environment around the infected person. Therefore, transmission of the COVID-19 virus can occur by direct contact with infected people and indirect contact with surfaces in the immediate environment. Published data have suggested that sneezing may produce as many as 40,000 droplets between 0.5–12 μm in diameter that may be expelled at speeds up to 100 meters/second whereas coughing may produce up to 3000 droplet nuclei, about the same number as talking for five minutes. Despite the variety in size, large droplets comprise most of the total volume of expelled respiratory droplets.
Airborne transmission is different from droplet transmission as it refers to the presence of hundreds of viruses within droplet nuclei filled with many viruses from an infected individual, which are generally considered to be particles <5μm in diameter, that can remain in the air (aerosol cloud) for long periods of time and be transmitted to others over distances greater than 6 feet. Think of an invisible cloud of tiny particles suspended in the air inside a room with poor ventilation. Remember it may take only a few hundred viruses to create an infection and there are hundreds of viruses in a single respiratory particle.
Blumberg and William Ristenpart, a professor of chemical engineering at UC Davis, go on to explain how the virus spreads and how to prevent transmission.
Transmission by droplets.
The expelled droplets are about one-third the size of a human hair but still large enough that we can see them. Masks create an effective barrier against droplets. “Everyone should wear a mask,” Blumberg said. “People who say, ‘I don’t believe masks work’ are ignoring scientific evidence. It’s not a belief system. It’s like saying, ‘I don’t believe in gravity.’ Blumberg goes on to say, “People who don’t wear a mask increase the risk of transmission to everyone, not just the people they come into contact with. It’s all the people those people will have contact with. You’re being an irresponsible member of the community if you’re not wearing a mask. It’s like double-dipping in the guacamole. You’re not being nice to others.”
Transmission by aerosol particles.
Droplet nuclei transmit COVID-19 via the tiny aerosol particles we expel when we talk forming the viral cloud we mentioned earlier. Those are about 1/100th the size of a human hair and are more difficult to defend against. Ventilation likely plays an important role in how easily the virus can be transmitted through the air. Indoor spaces probably pose a higher risk than outdoor ones, especially if they are poorly ventilated. Crowded areas such as bars, restaurants and subway trains could all be risky—especially if people are asymptomatic and spend long periods of time in such areas. Precautions could include better ventilation, regular cleaning and mask wearing. Therefore, staying outdoors with appropriate social distancing where there is more air flow is the best bet.
“Studies in laboratory conditions now show the virus stays alive in aerosol form with a half-life on the scale of hours. It persists in the air,” Ristenpart said. “That’s why you want to be outdoors for any social situations if possible. The good air flow will disperse the virus. If you are indoors, think about opening the windows. You want as much
fresh air as possible. “This is why, he said, places like bars are particularly hazardous for aerosols, on top of the likelihood of minimal distancing. “The louder you speak, the more expiratory aerosols you put out,” he said.
Additional topics:
The plexiglass shields in stores and restaurants only help somewhat. The same is true for office cubicles. After a time, transmission is possible from aerosols if the air flow is not good. “The way to think about that is to think about smells,” Ristenpart said. “If the person on the other side of a cubicle or plexiglass is wearing perfume, eventually, you’ll smell it. The aerosol particles are small enough to travel on air much like aromas. That’s why air flow is so important, along with other actions like wearing masks and social distancing.”
“If you’re going past someone very quickly in a grocery store,” Blumberg said, “the risk of getting infected is very low. It’s really lingering and talking that does it.” Ristenpart added: “It’s really important to know that just because you’re standing 6 feet or 7 feet away, if you have a prolonged conversation, there is still a risk. These aerosols can be carried along on weak air currents.”
There is no precise research on the prevalence of transmission from hand contact. “For ethical reasons, we can’t contaminate a bunch of people’s hands, then have them touch their faces or other people’s faces,” Ristenpart said. “But backtracking infections and following transmission events shows surfaces or hand contacts are not a primary method.” Which brings researchers back to droplets and aerosol particles as the primary methods of transmission.
“We know from other coronaviruses that this is primarily a respiratory transmitted illness,” Blumberg said. “There is a very small chance of transmission via groceries or mail or things like that. But washing hands is still always good.”
Children are less likely — by half — to be infected if they are exposed, less likely to be symptomatic and less likely to have a severe case if they do get sick, Blumberg said. “They appear to be less likely to infect others,” he said. “This is different from other infections like the flu when they are carriers. This appears to be much more of an adult disease. But children can still get sick and can still transmit it to others, so it’s important to be as hygienical with them as their development allows.”
Connecting the research.
Both scientists said the evidence has become even more powerful for wearing masks and social distancing. For instance, research shows that about 30 percent of infections are caused by people who do not know they have COVID-19 because they are asymptomatic or their symptoms have not appeared yet.
“So we don’t know who might spread it,” Blumberg said. “We do know social distancing reduces the risk of transmitting the virus by 90 percent, and wearing masks decreases the risk by 65 percent.
“Wearing a mask affects everyone,” he said. “If you care about your family or friends, or if you care about your community, wear a mask.”
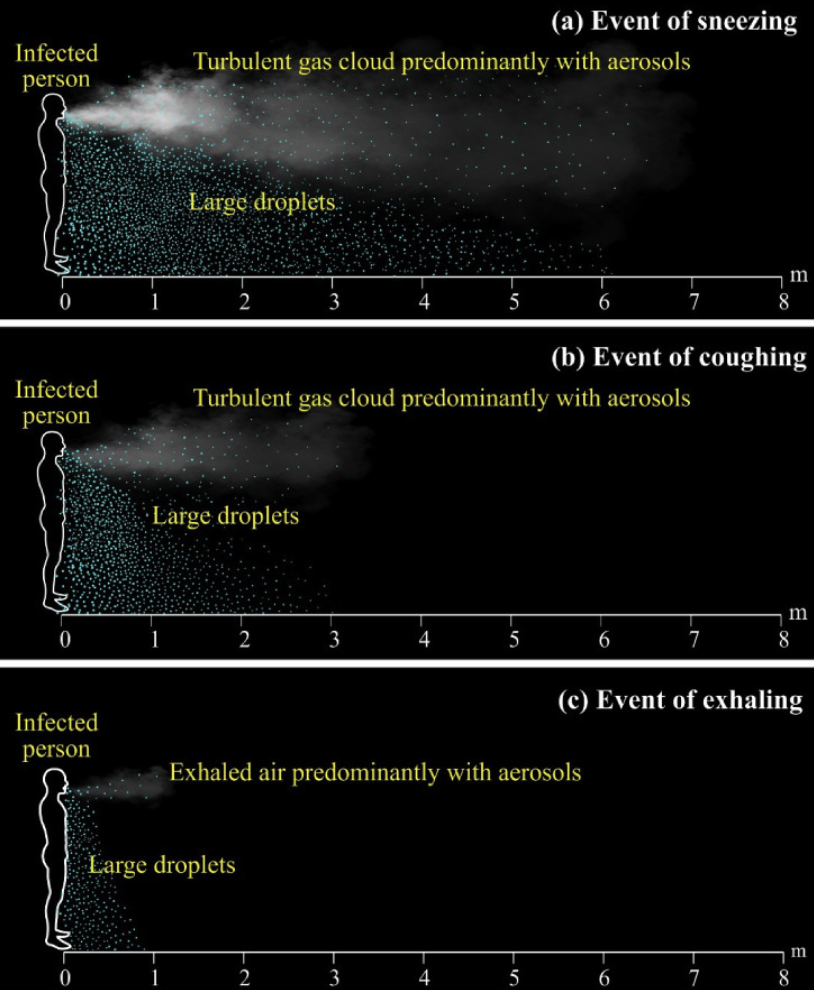
You can view the two illustrations below to better understand how masks can control the spread of disease. The first illustration demonstrates the relative production of both large droplets falling to the ground within 6 feet as well as the generation of an aerosol cloud from smaller droplet nuclei from actions such as sneezing, coughing and exhaling.
This second illustration demonstrates the relative protection of various types of masks compared with no mask at all.

Natural Hazards: Stingrays
At our Urgent Care office in Pacific Beach we often see patients with injuries incurred on the sand or in the ocean. Surfers present all year with lacerations caused by a board that got away from them.
But in the summer and early fall, when the ocean water temperature is at its warmest, we regularly see patients who have unexpectedly come upon a stingray in the ocean. These creatures spend their time on the ocean floor, commonly in shallow waters and near the jetties. Most injuries occur when the surf is small and the waters more calm. It seems that is when the Stingrays like to venture out and search for sand crabs and snails. Easy to see why humans entering the ocean would be seen as a predator to them. Their reaction is to fling up their tail in defense which contains venomous barbs. These barbs, which can cause a puncture wound or laceration, also result in substantial pain.
Lifeguards are quite adept at starting treatment for stingray injuries, which is soaking the affected body part, most often the foot or ankle, in a bucket of warm water. While some patients treat these injuries at home, many come to the Urgent Care where we will continue to soak the affected area in very warm water of about 105 to 115 degrees. In addition, we will check for the possibility of a retained piece of the barb, help to control any bleeding and provide a Tetanus shot if immunization is not up to date.
It’s important to keep the wound clean and covered initially and to keep an eye out for infection. We sometimes need to prescribe antibiotics to the small percentage of those whose wound becomes infected.
Don’t let the possibility of coming across a stingray keep you away from enjoying our beaches! Just be mindful of when you are most likely to encounter a stingray: in warm, calm waters. Another way to avoid stingray encounters is to shuffle your feet when they are on the ocean floor. This will alert the stingray of your proximity and allow them to move upward, away from you. This prevents you from stepping on one, encountering the defensive flip up of the tail and an unexpected injury.
San Diego Sports Medicine Urgent Care is located at 1945 Garnet Avenue in Pacific Beach. We love the San Diego community including the round stingrays that are part of our local wildlife. Click on the photo below to view one of these Del Mar residents getting a snack from a local kayaker.
Boosting Your Immune System
Over the past few months you may have heard quite a lot about your immune system. How our bodies respond to viral particles of COVID-19 and how we may improve our resistance to it. We’ve covered a few ways to boost your immune system in past newsletters, and in the coming weeks we will take one aspect of immune health and dive a bit deeper. We’ll share practical tools and purposeful habits you can incorporate into your daily life. Whether it’s COVID-19, the coming flu season, cancer, or autoimmune disease, a healthier immune system is central to a long and healthy life!
The Effect of Exercise on Immunity
The immune system is a complex network of specialized cells and proteins that protect our bodies from bacteria, viruses and other pathogens. It is also responsible for repairing cells, tissues, and reduces inflammation. Exercise is just one lifestyle habit that has been found to improve both the ‘fighting’ and the ‘repairing’ sides of the immune system.
We know that social isolation and confinement have negative effects on our immunity. These conditions can create stress that results in cortisol which not only increases inflammation and negatively impacts the immune system, but also alters appetite, sleep, and moods. This is particularly important to address now as social distancing measures may be necessary for some time.
Exercise slows the release of the hormone and promotes the production of billions of specialized immune cells throughout the body. In particular, cardiovascular exercise stimulates the release cytokines IL-6, IL-7, and IL-15 from the muscles. IL-6 can direct immune cells toward an infection, while IL-7 stimulates new T-cells, and IL-15 promotes NK, or natural killer cells, that dispose of infected cells. Exercise induced IL-15 has other roles including regulation of visceral or abdominal fat and anti-tumor activity.
While one exercise session may give your immune system a temporary boost, it is believed that regular exercise provides the most benefit. According to the American College of Sports Medicine, those who get regular exercise and have higher age and sex-adjusted scores for cardiorespiratory fitness show improved immune responses to vaccination, lower chronic low-grade inflammation, and improve various immune markers in several disease states including cancer, HIV, cardiovascular disease, diabetes, cognitive impairment and obesity. Theories on how exercise supports the immune system include:
- Flushing bacteria out of the lungs and airways. This may reduce your chance of getting a cold, flu, or
other illness. - Changes in antibodies and white blood cells (WBC). WBCs are the body’s immune system cells that fight disease. These antibodies or WBCs circulate more rapidly, so they could detect illnesses earlier than they might have before.
- The brief rise in body temperature during and right after exercise may prevent bacteria from growing.
- This temperature rise may help the body fight infection better. (This is similar to what happens when you have a fever.)
- Exercise slows down the release of stress hormones. Some stress increases the chance of illness. Lower stress hormones may protect against illness.
Stay safe San Diego!
SDSM continues to be available to help you. With telemedicine or an in-person visit, we can meet your needs for general physicals, annual health assessments, management of chronic conditions, and treatment of injuries. You can trust that we disinfect between each patient interaction and ongoing throughout the day. Cold/flu/COVID-19 symptoms and patients at increased risk of complications from COVID-19 are still best addressed through a convenient telemedicine appointment, as are on-going treatment assessments and check-ins with your provider.
Please call us if you feel ill, especially if you have diabetes, asthma, COPD, heart problems, impaired immune function, difficulty getting enough sleep, or are experiencing high levels of stress. Working together, we can help you to stay healthy and thrive.
Yours in health,
The Physicians and Staff of San Diego Sports Medicine and Family Health Center

