COVID-19 Vaccines and Blood Clot Risk 
by Tess Maloney, FNP-C
The FDA and CDC have approved the use of the Johnson & Johnson/Janssen COVID-19 vaccine in the U.S. after a temporary pause. A small number of cases of serious blood clots in the setting of low platelets occurred in women under 60 after receiving the J&J vaccine. A review of all available data at this time shows that the known and potential benefits of the J&J/Janssen vaccine outweigh its known and potential risks. The reason for the pause in the administration of the J&J vaccine was to sort out risk factors for the clotting problem, known as thrombosis with thrombocytopenia syndrome (TTS), and to determine the best treatment, which for these specific clots is different than using typical blood thinners. This process demonstrates the safety systems for vaccines are working as they should to catch potential issues. The CDC and FDA will continue to monitor the safety of all COVID-19 vaccines.
The Johnson & Johnson COVID-19 vaccine is a one dose viral vector vaccine. If you have received this vaccine and develop symptoms such as severe headache, blurred vision, persistent abdominal pain, shortness of breath, chest pain, leg swelling, easy bruising or tiny blood spots under the skin, especially within three weeks of receiving the vaccine, seek prompt medical care. If you received the J&J vaccine over three weeks ago, there is much less concern about clotting.
There have been no reports of TTS with the Pfizer-BioNTech or Moderna mRNA vaccines.
References
1. CDC J&J/Janssen Vaccine Update
2. CDC Vaccine Product Information
3. CDC and FDA Statement on J&J Vaccine
4. Cases of Cerebral Venous Sinus Thrombosis with Thrombocytopenia after Receipt of the Johnson & Johnson COVID-19 Vaccine
5. Thrombotic Thrombocytopenia after ChAdOx1 nCov-19 Vaccination
6. Thrombosis and Thrombocytopenia after ChAdOx1 nCoV-19 Vaccination
7. Tang N, Bai H, Chen X, Gong J, Li D, Sun Z. Anticoagulant treatment is associated with decreased mortality in severe coronavirus disease 2019 patients with coagulopathy. J Thromb Haemost. 2020 May;18(5):1094-1099. doi: 10.1111/jth.14817. Epub 2020 Apr 27. PMID: 32220112.
The Road to Becoming a Fellow 
By Alexandra Myers, D.O.
Have you ever seen some extra letters after your doctor’s name? Well, those extra letters usually mean that your doctor has spent extra time to become an expert in their field of practice. I was recently honored with the distinction of Fellow of the American Osteopathic Academy of Sports Medicine, and so will be adding the letters FAOASM to my credentials. This is an award given to physicians who have practiced sports medicine and have been active in caring for elite athletes, as well as teaching their colleagues and students on the advancement of sports medicine.
A physician’s education begins in medical school after which they must complete a residency. When a physician graduates from their residency training, they usually complete a process to become Board Certified (BC) in their field such as in Family Practice or Internal Medicine.
The physicians at San Diego Sports Medicine and Family Health Center have taken additional formal education following residency training in their Primary Care specialty (Family Medicine or Internal Medicine) and have earned Board Certification in Sports Medicine (the exception is Dr Cheffet who is residency trained in both Internal Medicine and Pediatrics). Many of our doctors are also leaders within their professional organizations. Four of our doctors have become President of their specialty college or risen to presidency of our state specialty organizations. No matter the chosen path, each year, our doctors spend many hours completing continuing medical education (CME) in order to stay up to date on their knowledge and provide excellent care.
I am proud to be joining these esteemed physicians who have also attained Fellowship status within our professional organizations.
Dr. Richard Parker – Fellow of the American Osteopathic Academy of Sports Medicine
Dr. Jeff Anthony – Fellow of the American Academy of Family Physicians, Fellow of the American Osteopathic Academy of Sports Medicine
Dr. Allen Richburg – Fellow of the American Academy of Family Physicians
Dr. Michelle Look – Fellow of the American Academy of Family Physicians
Dr. Steve Rohrer – Fellow of the American Osteopathic Academy of Sports Medicine
Dr. Shannon Cheffet – Fellow of the American Board of Pediatrics
Dr. Lee Rice – Fellow of the American Osteopathic Academy of Sports Medicine, Fellow of the American Academy of Family Physicians, Fellow of the American Medical Society for Sports Medicine
Should You Still Take Zinc?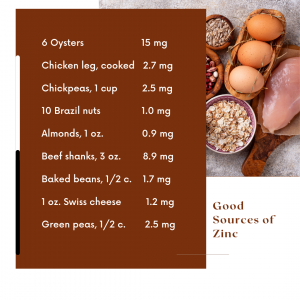
By Linda Illingworth, RDN
Well over a year has passed since the immune system became a focus in prevention of COVID-19. Zinc was among the nutrients most often recommended, but if you have been consistently supplementing with zinc for months on end, it may be time to take a break.
Minerals are essential for our health yet are needed in very small quantities. They have unique roles in our body and are most often catalysts for important processes like the production of energy, muscle contraction, and nerve transmission. Many of them compete for absorption in the digestive tract. For example, calcium and magnesium compete for the same absorption site, and zinc can interfere with copper and iron absorption.
In the case of zinc, a copper deficiency can occur with long term or high dose supplementation. Large amounts of zinc can also impact the bioavailability of iron and lead to anemia in those with low or marginal iron stores. The RDA for zinc is 11 mg per day for men and 8 mg per day for women. Historically, the RDA was 15 mg per day but was reduced in 1980. The current RDA was based on the absorption of a stable zinc formula rather than zinc from a mixed diet. So it has been suggested that the zinc requirement may be 50% greater than the current RDA. Nonetheless, it is not advised to take supplemental zinc in excess of the RDA in perpetuity. It is safer to focus on food sources of zinc and limit supplemental zinc to15-20 mg per day. If you have been consistently taking a zinc supplement the argument could be made that your zinc status is adequate, if not stellar, and food sources alone can provide enough going forward.
Good food sources of zinc include oysters, beef, chicken, chickpeas, Brazil nuts, fortified cereals like Total, and whole grains. Many plants contain phytates which can form a complex with zinc and prevent its absorption. Soaking or sprouting grains and nuts before consuming helps reduce phytic acid and enhance absorption. In addition, both baker’s yeast and sourdough contain enzymes that lower phytate content making zinc and other minerals more bioavailable. It is also thought that the fibers found in fruits and vegetables may also bind zinc contributing to a decrease in absorption. Those most at risk of zinc deficiency are young children, pregnant women, vegetarians due to the higher intake of phytates, adolescent vegetarians, people with liver disease, alcoholism, Alzheimer’s, and those on hemodialysis.
Check out the foods high in zinc and see if you can’t get 10 or more milligrams each day. Review your supplements and adjust your intake if needed. If you have more questions on zinc drop us a line at news@sdsm.com.
References:
1. NIH: Office of Dietary Supplements, Consumer Information for Zinc
2. Armah SM. Fractional Zinc Absorption for Men, Women, and Adolescents Is Overestimated in the Current Dietary Reference Intakes. J. Nutr. 146(6):1276-80. Jun, 2016
3. Arendt EK, Ryan LA, Dal Bello F. Impact of sourdough on the texture of bread. Food Microbiol. 2007 Apr;24(2):165-74. doi: 10.1016/j.fm.2006.07.011. Epub 2006 Sep 20. PMID: 17008161.

